Here at MPN, we see many cases of liver disease. If your pet has been given the diagnosis of liver disease and you want the very best for them, then read on. Feeding prescription diets don’t often work successfully and if you want to learn about how you can help with fresh food and supplements, then this is the guide for you.
Liver disease can present differently, so I have listed some of the common disease we see today.
Chronic Hepatitis is the most common primary liver disease found in dogs. This chronic inflammatory condition is generally not determined although genetics, copper, infectious agents, infections such as leptospirosis or viral infections, severe trauma and various drugs (phenobarbital, NSAIDs, paracetamol) may be implicated. Copper-associated hepatitis, where copper accumulates within hepatocytes can become toxic and cause liver damage.
Acute liver failure results in sudden loss of liver function, which is often associated with neurologic problems and blood clotting issues. It can occur due to a sudden injury or due to an additional issue, taxing an already diseased liver.
Hepatic encephalopathy, a syndrome of neurologic problems caused by poor liver function, is seen in a quite a few liver disease cases. While the development of this condition is not totally understood, failure of the liver to clear poisons from the bloodstream, changes in amino acid metabolism and neurologic issues may synergistically work together to cause this disease.
Portosystemic shunts are often described as congenital (inborn). However, they can rarely develop over time due to illness and this is called an acquired liver shunt (often occurring in older dogs and less frequently in cats). They can be caused by high blood pressure in the vessels entering into the liver. In a healthy cat or dog, blood supply draining the intestines, travels through the portal vein into the liver, where it is then filtered. It then returns blood to the heart via the vena cava. A portosystemic shunt (also known as PSS), is an abnormal vein connecting the blood supply returning from the intestines to the vein returning blood to the heart. It bypasses the liver by shunting the blood flow and there in lies it’s name.
The key is to detect liver disease early as it can take months or even years to identify itself.
There are number of signs and symptoms in Liver Disease. If any of these arise consistently, you should go to the vets and get it checked out.
Unfortunately, the majority of these aren’t necessarily specific to liver disease as signs and symptoms can vary from case to case. A visit to the vets as soon as any symptoms arise, is always the best option.
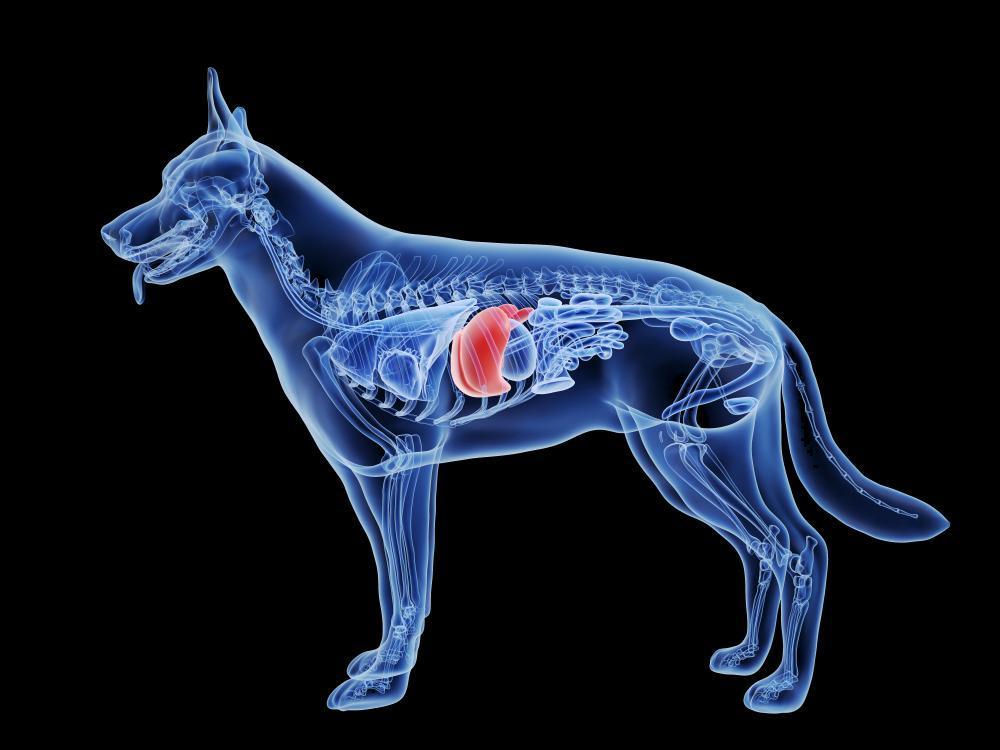
I refer to the liver as the power house. It manages, processes and filters pretty much everything in the body.
The liver has two main sections, called the right and the left lobes. The gallbladder sits under the liver, along with parts of the pancreas and intestines. The liver and these organs work together beautifully to digest, absorb, and process food.
The liver filters the blood coming from the digestive system, before passing it to the rest of the body. The liver also detoxifies chemicals and metabolises hormones and drugs and any other toxins the body needs to rid.
Whilst all of this is going on, the liver secretes bile that ends up in the intestines, emulsifying fats in the digestive process.
The liver also makes proteins essential for blood clotting and many other functions.
Its an incredibly clever and intuitive organ and can even regenerate liver cells, even if a portion of liver is removed in surgery. It’s a miraculous organ and your pet relies on it’s functioning for good health.
Poor Diet; can trigger genetics and put a massive strain on the liver. Diet may not be solely responsible in the etiology of this disease, but it certainly plays a role in treatment and support.
Stress; should never be underestimated in the pathogenisis of liver disease. Trying to modulate the stress response is always helpful in any disease state.
Copper Toxicity; copper-associated hepatitis, where copper accumulates within hepatocytes can become toxic and cause liver damage. This can be due to a low level zinc diet or genetics that impair the detoxification of copper and the assimilation and absorption of zinc.
Low Copper
Endocrine Disease; diabetes mellitus, hyperadrenocorticism (Cushing’s disease) and hyperthyroidism are all diseases in which impaired liver function can arise. i always ask for your vet to check this first, as treating the underlying endocrine disease is often the most important and effective part of caring for the liver.
Infectious agents (leptospirosis or viral); sometimes vets will say the cause of liver disease is unknown but testing for a viral infection can sometimes implicate liver damage. We find working with the immune system in these cases and supporting the liver function is essential. Several types of infections may affect the liver, including bacterial, fungal, and parasitic diseases.
Severe trauma; your pet could have been in a terrible accident that involved the liver area. Trauma can cause damage so understanding that trauma is important.
Pharmaceuticals; the overuse or poor tolerance of phenobarbital, NSAIDs, paracetamol and other drugs may be implicated in liver disease.
Vaccinosis; we are keen on safe vaccinations. We adhere and recommend the WSAVA vaccination guidelines as a minimum (world small animal veterinary association). MPN promote titer testing over vaccinating yearly and 3 yearly, due to the potential immune impact on genes, detoxification and health.
A variety of blood tests can be used in detecting and diagnosing liver disease. Mostly blood tests of liver enzymes can establish is something is going on. X‑rays and ultrasonography can further help your vet determine liver size, irregularities, damage, gallstones, and diseases of the gallbladder.
Abdominal surgery is common and is considered the treatment of choice for extrahepatic portosystemic shunts (PSS).
A prescription diet with low fat and low protein is often prescribed to your beloved pet regardless of the type of liver disease. Some vary in sodium content, some may contain extra zinc for copper toxicity but they are mostly developed with the same approach of not overtaxing the liver with fat or protein metabolism.
We don’t recommended dry food in liver disease. Fresher and more bioavailable, lean proteins may be more effective as the liver doesn’t have to work so hard in metabolising these macronutrients. The protein in dry food can be cross-linked and not easily assimilated. Quality and digestibility of food is one of the most important factors in managing liver disease. Also, dry food can contain anywhere from 30-70% carbohydrates from the many starch containing ingredients.
Fats are usually our biggest consideration in liver disease. On a wet basis we tend to feed anywhere from 2-7% but ideally around 4-5%. On a dry matter basis we look for 10-15%. Lean proteins, good vegetables, superfoods and the like are ideally what we base our formulas on. Obviously each case is different but in the checklist above, you can see there are some clinical parameters we would always work to.
Low Fat VenisonRestricting dietary protein is controversial as testing and research was mostly based on processed food, fed to cats and dogs with limited solid findings. There isn’t a clear consensus as to what level protein intake should be reduced to in the diet of pets with liver disease but we find moderate levels of fresh and more bioavailable proteins, slightly lower in phosphorus (in the case of liver shunts), is always the way to go. MPN always work with liver enzyme blood tests to check markers to gauge the severity of each case.
Protein is needed to support hepatic regeneration and prevent negative nitrogen balance. In a healthy animal, protein in excess of the body’s needs is deaminated, the carbon chain used for energy or stored energy and the nitrogen converted to ammonia. The ammonia is then converted to urea by the liver and urea excreted by the kidneys. In animals with liver failure, the conversion to urea is decreased and excess nitrogen may cause increased ammonia, one of the toxins involved in hepatic encephalopathy (HE).
The type of protein you feed a cat or dog with liver disease should also be considered. Protein with high biological values leaves less waste behind.
Good proteins to feed for liver disease are eggs for the most bioavailable protein and choline content, poultry and a little fish such as sardines, salmon and cod.
Other proteins to include would be lean meats such as venison, ostrich and kangaroo. If we need to reduce phosphorus and fats, tripe is a wonderful addition to the diet. Red meats are generally higher in fat and often best avoided.
Complex Carbohydrates in grain form are something we tend to avoid with cats and dogs. If we are in need in reducing protein we may consider quinoa or oats but only if necessary.
We do however love the starch rich vegetables such as sweet potato and in particular purple sweet potato in liver disease. In juice form, this beautiful vegetable in a Japanese study, helped to reduce raised liver enzymes.
Green vegetables such as broccoli, kale and brussell sprouts have shown to reduce fatty build up in the liver during disease. Broccoli contains glucobrassicin, the glucosinolate precursor of indole-3-carbinol (I3C) and subsequently Diindolylmethane (DIM) which is attributed to supporting phase one of the liver detoxification.
Low Fat Kangaroo
Berries and cranberries whole and in extract contain anthocyadins that demonstrate hepato-protective abilities. An experiment found that antioxidants commonly found in berries slowed the development of lesions and fibrosis, the development of scar tissue, in the livers of rats.
It’s recommended that sodium levels should be restricted moderately. This is because excessive levels of sodium can over work the liver but still required for other important bodily functions. Sodium and trace minerals are always better received from whole foods and healthier versions of salt such as Himalayan.
Fats such as omega-6 and omega-3 in 4:1 ratio is important in liver conditions. Moderate amounts on hemp oil, phytoplankton (offering DHA and EPA) and fish whole and in pure oil source may help to protect the liver and reduce systemic inflammation and inflammation in the liver.
The addition of some fibre helps to speed up colonic transit and prevent constipation. This allows toxins less chance to be absorbed from the colon and circulated into the system for the liver to deal with.
Treats and tidbits are fine for cats and dogs with Liver Disease as long as they fit the dietary criteria and don’t exceed the daily feeding amount.
Always filter or provide fresh bottled water for your pet. Tap water contains flouride, pesticides, fungicides and many more toxins that the liver must process during detoxification. To keep things more interesting a broth could be a great alternative to water. However, be careful the broth doesn’t contain high levels of sodium. Even a little liquid chlorophyll in water can be helpful for electrolytes and has shown to help with high levels of ammonia in the body.
Ashwaganda; quite often liver function can be affected by the endocrine system and intense levels of stress. I find most dogs experience some form of stress living in our 21st century homes under our rules. Ashwaganda is one of the most important herbs in Ayurveda, a form of alternative medicine based on Indian principles of natural healing that has been used for over 3,000 years. It’s a beautiful adaptogenic herb that supports the stress response and immunity in your pet. It’s classically known as a nervine tonic but this beauty has many strings to its bow. The clinical studies and research so far is very promising. This herb can have an indirect impact on liver function in a very positive way.
B vitamins: such as methylated forms of folate (B9) and cobalamin (B12) are essential in this case. A B complex is best to support Liver function. B1 and B9 for methylation are key in sulfation pathways in the liver detoxification process. Choline is also included in this complex. Choline deficiency can be created in experimental animals and causes fatty liver, which is often used as an experimental model for fatty liver disease. Whether choline deficiency is an important cause of fatty liver disease is not known, but severe protein-calorie malnutrition is often accompanied by marked fatty liver and choline supplementation of total parenteral nutrition decreases fat accumulation in the liver. I often find food alone doesn’t offer enough support of the B vitamins and especially B9.
Probiotics; Your dogs microbiome is as individual as they are. Microbiome is a community of thousands of different diverse bacteria, fungi and virus, all working together to fuel health and immunity. Gut microbiotia is essential in health and driven/affected by diet, stress, environmental conditions and so on. Probably the most important bacteria phylum in your dog is Bacteroidetes. These bacteroidetes produce short chain fatty acids that help balance immunity and also help prevent leaky gut syndrome. Microbiology on your pet’s poop can really tell us a lot and allow us to add in the correct bacteria or alter diet accordingly. We know the liver and efficacy of the digestion are closely correlated so a healthy bowel can reduce the stress and impact of a healthy or unhealthy liver. Research now demonstrates that the gut microbiome can impact the health and functioning of the liver.
Curcumin BCM-95 ®; is the active ingredient in turmeric, found in the roots and bulbs of the Curcuma longa plant. There are over 6,000+ published studies on turmeric and namely curcumin the compound that is an antioxidant, anti-inflammatory, antiviral, antibacterial, anti fungal, and with possible anticancer properties or at best support. Oxidative stress has been considered a key causing factor of liver damage induced by a variety of agents such as virus, injury, genetics, pharmaceuticals and so on. Curcumin is one of the most commonly used indigenous compounded herbs that demonstrates various functionalities in protecting the liver.
Omega-3 fatty acid: the potential consequences of an alteration in the ratio of omega-6 to omega-3 fatty acid consumption (often outrageously high in dry fed/grain rich pet foods over 20:1) are increased production of pro-inflammatory arachidonic acid-derived eicosanoids and impaired regulation of hepatic and adipose function that. I prefer certain types of clean fish oil such as sardines and algae oil. Frozen sardines are better than canned as this can pose mercury problems if fed frequently. a careful approach to using fats is always advised but can be beneficial. I like to use pure and emulsified omega fats on the market to take the pressure off the liver during fat digestion involving the liver and gallbladder.
Fat-soluble vitamins (A,D,E,K); any disorder that decreases the amount of bile acids entering the intestine can interfere with intestinal fat absorption. This can reduce the uptake of the fat-soluble vitamins A, D, E, and K. Asking your vet to check these is important in liver disease. Vitamin D and E are often indicated in liver disease. These should be supplemented under a professional.
Zinc; high copper toxicity can be due to a defect in the biliary excretion of copper, which is the main control of copper balance in the liver. Zinc in nature works in synergy with copper and so low levels of zinc can raise copper levels. Likewise if a good amount of zinc is supplemented in the diet, this can chelate (pull out and prevent further issues with copper). Zinc is the second most important mineral in your dog’s body although studies show that only 15–40% of ingested zinc from diet is actually absorbed. Natural and commercial diet’s can naturally be low or lacking in zinc but if your dog has a malabsorption issue with zinc (common in huskys) this problem of deficiency can become very real.
SAMe (S-Adenosyl-L-Methionine); SAMe supplementation shows to restore hepatic glutathione (GSH) deposits and aids support in liver injury. SAMe is part of the methionine cycle in creating a methyl donor for methylation (a process that allows 1000’s of biochemcial pathways to be fulfilled in the body). This can only be obtained from veterinarians in the U.K. Research shows some inconclusive data but in my experience it can work well under supervision.
N-Acetyl Cysteine; NAC is a precursor of the amino acid L-cysteine that supports glutathione elevation biosynthesis. It acts directly as a scavenger of free radicals, especially oxygen radicals associated with the liver. Supplementing dogs with N‐Acetyl Cysteine (NAC) helps to increase cysteine levels, normalising glutathione concentrations, and decreasing the degree of lipid peroxidation associated with liver disease.
Milk Thistle; the milk thistle plant stimulates liver repair and detoxification through four main avenues: 1. antioxidation, free radical scavenging and glutathione regulation; 2. stabilization of cell membranes and permeability, which limits hepatotoxin entry into hepatocytes; 3. ribosomal RNA synthesis promotion, stimulating liver regeneration; and 4. slowing transformation of stellate hepatocytes into myofibroblasts, slowing the onset of cirrhosis arising through collagen deposition.
Toxins that put a stress on the body and liver are a plenty in your pet’s life. If a cleaner lifestyle can be adopted, this is best to protect liver function. Avoiding flea and tick treatments, dewormers, heart worm drugs (if possible), can take a burden off the liver and support detoxification pathways.
– Wormcount companies: www.wormcount.com OR www.feclab.co.uk
– Look to titer testing rather than yearly vaccines (checkout Vaccicheck)
– Question your vet on the medications currently being given to your pet, are they necessary. Reducing pharmaceuticals (if possible), means you can lighten the load on the liver
In summary, a fresh low fat diet with supplements for liver disease is a great way to hopefully prolong survival and improve quality of life. In general, damage done to the liver, if far advanced, can’t necessarily be reversed but there are many things you can do to support function. Prevention and detecting disease in early stages is key.
Seeking professional advice is always recommended.
If you want to find out more, check out our consultation services.
Thanks for reading folks.
MPN Team